Progress notes are an important tool in tracking and monitoring the progress of patients receiving medical or psychiatric care. They are essential for documenting changes in a patient’s behavior, mood, and physical condition, as well as noting any treatments or interventions that have been prescribed.
Common Elements in Progress Notes
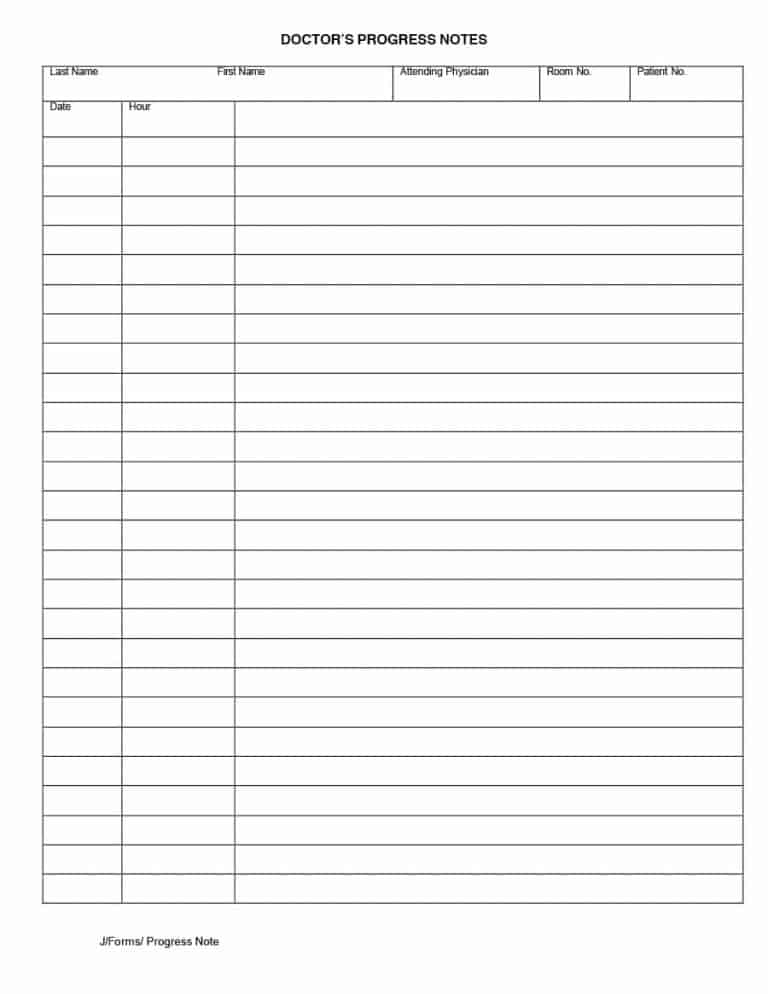
Regardless of the specific field of healthcare, there are certain common elements that are typically included in progress notes. These include:
- Patient identification information, including name, date of birth, and medical record number
- Date of the progress note
- A brief description of the patient’s symptoms and overall condition
- Details about any medications or treatments that have been prescribed
- Notes on any changes in the patient’s condition since the previous progress note
- Assessments of the patient’s mental health or physical health status
- Any other important information that may impact the patient’s care, such as family dynamics or social support systems
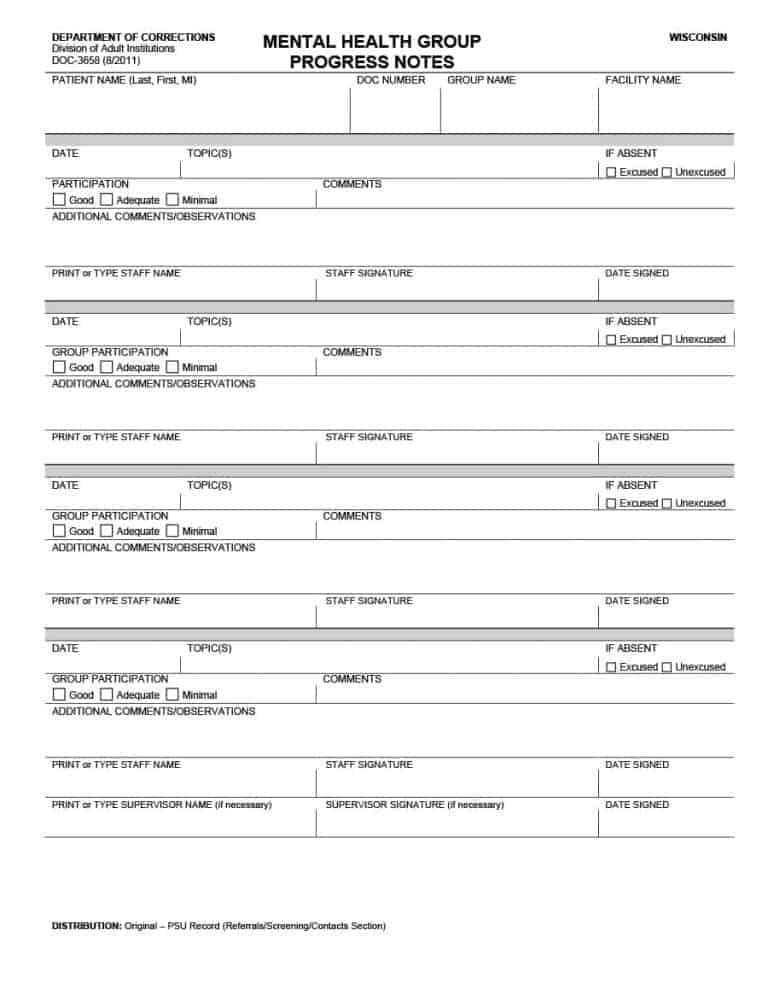
 Mental Health Progress Notes
Mental Health Progress Notes
In the field of mental health, progress notes are especially important for tracking changes in a patient’s mood and behavior. Mental health progress notes typically include:
- Details about any changes in the patient’s emotional state
- Information on the patient’s thoughts or feelings about their treatment
- Notes on any potential risk factors, such as suicidal ideation or self-harm behavior
- Any other relevant psychological information, such as past trauma or family history of mental illness
Psychotherapy Progress Notes
Psychotherapy progress notes are a type of mental health progress note specifically designed for use in therapy sessions. These notes may include:
- A summary of the session, including the main topics discussed and any breakthroughs or insights the patient may have had
- Details about any homework or exercises assigned to the patient during the session
- Notes on any challenges or obstacles that arose during the session, and how these were addressed
- Assessments of the patient’s progress towards their treatment goals
 Nursing Progress Notes
Nursing Progress Notes
In the field of nursing, progress notes are used to document a patient’s physical condition and any medical interventions that have been prescribed. Nursing progress notes may include:
- Details about the patient’s vital signs, such as blood pressure, heart rate, and temperature
- Notes on any changes in the patient’s physical condition, such as new symptoms or worsening of existing symptoms
- Information about any medical procedures or treatments that have been administered, including dosages and times
- Assessments of the patient’s pain level, and any interventions that have been undertaken to manage pain
- A summary of the patient’s overall progress, including any improvements or setbacks since the previous progress note
Benefits of Progress Notes
There are many benefits to using progress notes in healthcare settings. These include:
- Improved communication and coordination between healthcare providers, as progress notes provide a centralized, comprehensive record of a patient’s treatment history
- Clear documentation of the patient’s condition and treatment plan, which can help to avoid errors or misunderstandings
- Facilitation of research and data analysis, as progress notes can be used to identify trends or patterns in a patient population
- Protection against potential legal liability, as progress notes can help to demonstrate that appropriate care was provided
Best Practices for Writing Progress Notes
To ensure that progress notes are complete, accurate, and useful, it is important to follow certain best practices when writing them. These include:
- Completing progress notes in a timely manner, ideally within 24-48 hours of the patient encounter
- Using clear and concise language, avoiding medical jargon or abbreviations that may be difficult to understand
- Staying objective and factual, avoiding subjective evaluations or interpretations
- Ensuring that progress notes are HIPAA-compliant, meaning that they do not reveal any protected health information that could identify the patient
- Reviewing progress notes regularly to ensure that they are up-to-date and accurate
 Conclusion
Conclusion
Progress notes are a vital tool in healthcare settings, helping to ensure that patients receive appropriate and effective care. By documenting changes in a patient’s condition, noting any treatments or interventions that have been prescribed, and providing a centralized record of the patient’s care history, progress notes can help to improve communication between healthcare providers, facilitate data analysis and research, and protect against potential legal liability. By following best practices for writing and storing progress notes, healthcare providers can help to ensure that they are accurate, complete, and useful for patient care.